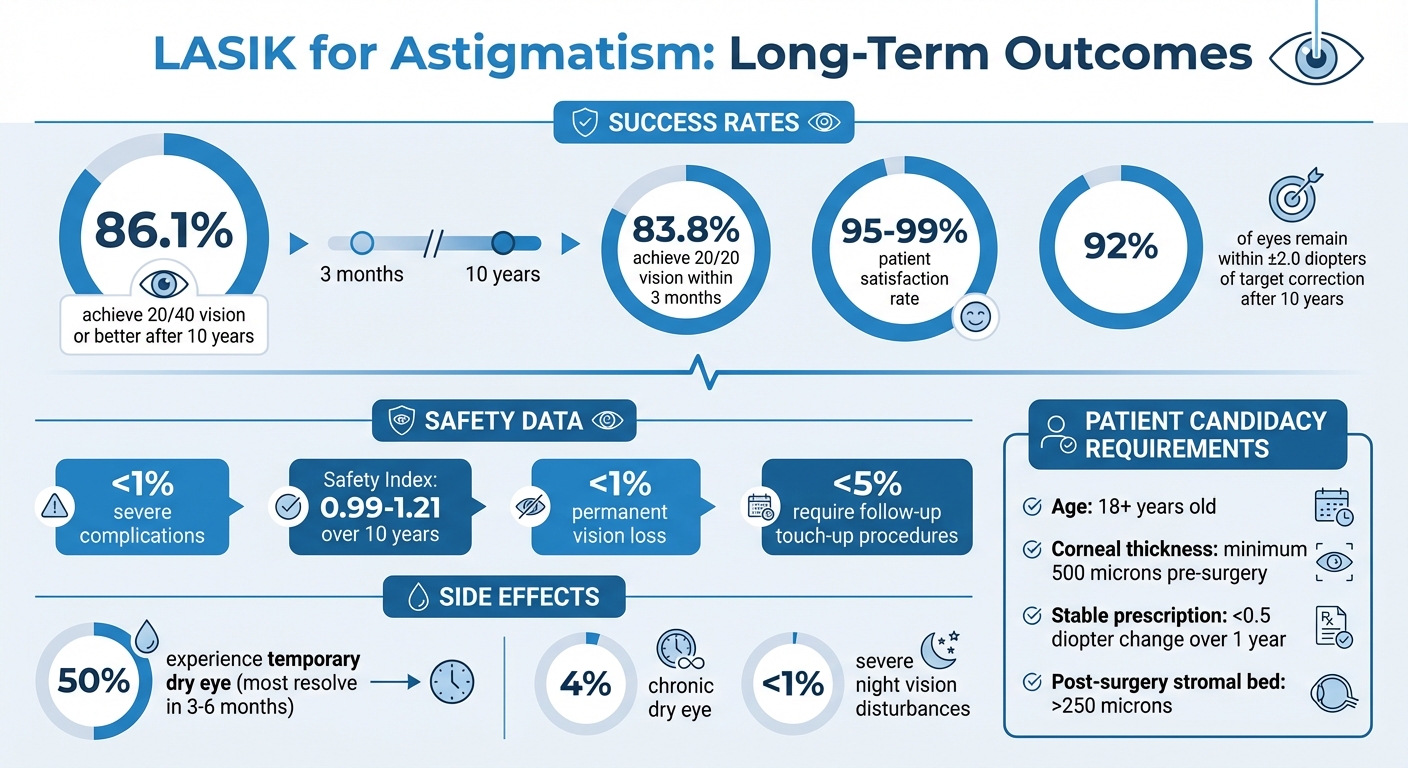
LASIK surgery offers a reliable solution for correcting astigmatism, providing lasting vision improvements for most patients. Studies show that 86.1% of patients achieve 20/40 vision or better after 10 years, and 95%-99% report satisfaction with their results. Safety data is reassuring, with severe complications occurring in less than 1% of cases, and modern advancements like femtosecond lasers and wavefront-guided technology have significantly improved outcomes.
Key takeaways:
- LASIK reshapes the cornea to correct astigmatism, with a success rate of 83.8% achieving 20/20 vision within three months.
- Long-term results remain stable, though slight vision changes may occur due to aging or natural eye development.
- Common side effects include temporary dryness (50% of patients) and rare night vision disturbances (<1%).
- Under 5% of patients require follow-up procedures for touch-ups.
Patients with stable prescriptions and healthy corneas are ideal candidates. Advances in technology, like iris registration and cyclotorsion control, ensure precise corrections. Proper post-surgery care, including using prescribed eye drops and attending follow-ups, is critical for maintaining results over time.
LASIK for Astigmatism: Long-Term Success Rates and Safety Statistics
Main Findings from the Long-Term LASIK Study
Study Design and Methods
Researchers have been closely monitoring LASIK outcomes over extended periods, with some studies spanning more than a decade. One such study, conducted at the Minami-Aoyama Eye Clinic in Tokyo, tracked 346 eyes treated for myopia and myopic astigmatism between December 1997 and February 2002. Another long-term study, led by Gracia Castro-Luna at the University of Almeria in Spain, followed 310 eyes treated with femtosecond laser-assisted LASIK (FS-LASIK) from 2008 to 2019. Both studies focused on LASIK’s ability to correct astigmatism, collecting data on visual acuity, refractive stability, and complications at regular intervals. These comprehensive approaches provided valuable insights into how patients’ vision evolved over time.
Vision Improvement Over Time
The results confirm that LASIK delivers lasting vision improvements. In the Tokyo study, 52.0% of patients achieved 20/20 vision, while 86.1% reached 20/40 or better after 10 years. The Spain study reported even better outcomes with FS-LASIK, showing that approximately 98% of patients maintained 20/40 vision or better at the five-year mark. Although a slight decline in visual acuity was observed over a decade – shifting from an average of -0.08 at one month post-surgery to 0.06 at 10 years – patients’ vision remained significantly improved compared to their pre-surgery levels. These findings highlight the procedure’s durability, but safety is just as critical.
Safety and Complication Rates
When it comes to astigmatism correction, patient safety is a top priority, and the data is reassuring. The Tokyo study reported a safety index of 0.99 at 10 years, while the Spain study recorded a higher safety index of 1.21 for FS-LASIK. Serious complications leading to permanent vision loss were exceedingly rare, occurring in well under 1% of cases. Temporary dry eye symptoms affected about 50% of patients, though only 4% experienced chronic dry eye. Night vision disturbances, such as glare or halos, were uncommon, with less than 1% of patients reporting severe or ongoing issues that interfered with daily life. Additionally, the need for follow-up enhancements was minimal, with rates typically under 5% for modern LASIK techniques.
What Affects Long-Term LASIK Results
Patient Characteristics
Long-term LASIK success is influenced by a mix of patient-specific factors and technological advancements. When it comes to individual characteristics, age plays a key role. Surgeons typically avoid performing LASIK on individuals under 18, as their eyes are still developing. On the other end of the spectrum, patients over 40 are more likely to need touch-up procedures later. In fact, about 10% of LASIK patients require enhancements, with those over 40 or those needing higher initial corrections being more prone to this.
Another crucial consideration is corneal thickness. For LASIK to be performed safely, the cornea needs to be at least 500 microns thick before surgery. If the remaining stromal layer after the procedure drops below 250 microns, it increases the risk of keratectasia, a condition where the cornea becomes dangerously thin. Astigmatism severity also affects outcomes. While only about 4.61% of people have moderate-to-high astigmatism (2.50 diopters or more), higher levels of astigmatism are harder to correct and can result in slightly less predictable results.
Your overall health is another factor that can impact healing. Conditions like uncontrolled diabetes, autoimmune disorders (e.g., Lupus or Rheumatoid Arthritis), or active infections can interfere with recovery and are often contraindications for LASIK. Additionally, having a stable prescription – defined as less than a 0.5 diopter change over one year – is essential for ensuring long-term success and minimizing complications.
Modern LASIK Technology
Advances in LASIK technology have dramatically improved long-term outcomes. One major leap forward is the use of femtosecond lasers to create corneal flaps. These lasers are more precise than traditional mechanical microkeratomes, allowing for thinner, more accurate flaps and reducing the risk of complications like corneal ectasia. This "all-laser" or bladeless LASIK approach is now the standard in most practices.
Another game-changing development is wavefront-guided technology, which creates a detailed 3D map of how light passes through the eye. This allows for the correction of both standard refractive errors and smaller visual imperfections. Dr. Steven C. Schallhorn from the University of California, San Francisco, highlights its effectiveness:
"Wavefront-guided LASIK for the correction of myopic astigmatism is safe, effective, and predictable."
To further enhance precision, modern systems use iris registration and cyclotorsion control to account for eye rotation during the procedure. Even a small misalignment – like 4° – can result in a 14% undercorrection, while a 10° misalignment can cause a 35% undercorrection. Additionally, newer excimer lasers use larger optical treatment zones and "blend zones", significantly reducing issues like glare and halos during nighttime.
Post-Surgery Care and Lifestyle Choices
How you care for your eyes after surgery also plays a big role in long-term results. In the first week, it’s important to use topical antibiotic and steroid drops four times a day to prevent infection and reduce inflammation. Preservative-free artificial tears are also critical for managing post-operative dryness, which affects about 50% of patients initially. Thankfully, most people notice improvements within 3 to 6 months.
Follow-up appointments are equally important. These typically occur at 1 day, 1 week, 1 month, and 3 months post-surgery to monitor the flap’s position, corneal health, and vision stability. During the early healing phase, avoid rubbing your eyes to prevent displacing the corneal flap. While LASIK results are generally stable, any vision changes over time are more likely due to natural aging – like presbyopia – rather than issues with the surgery itself. Studies show that 92% of eyes remain within ±2.0 diopters of the intended correction even a decade after the procedure.
LASIK Services at Cheyenne Eye Clinic and Surgery Center
Determining LASIK Candidacy
Cheyenne Eye Clinic and Surgery Center combines advanced technology with years of LASIK success to ensure patients get the best possible results. Before moving forward with surgery, the clinic conducts a thorough preoperative evaluation to determine if LASIK is right for you. This isn’t just a basic vision test – it’s a detailed process that includes cutting-edge 3D eye mapping. Using the iDesign Advanced WaveScan System, the clinic captures a precise blueprint of your eyes. This system employs a Hartmann–Shack aberrometer and a high-definition camera to measure both higher-order and lower-order aberrations, tailoring the procedure to your unique needs.
As part of the evaluation, the clinic’s surgeons carefully examine your corneal thickness and calculate the expected postoperative corneal stromal bed, ensuring it stays above the 250 μm safety threshold. They also screen for any active eye conditions, irregular corneal shapes, or medical issues that could affect healing. To qualify for LASIK, you need to meet specific criteria: you must be at least 18 years old, have stable vision (with less than a 0.5 diopter change in the past year), and be in good overall health.
If you wear contact lenses, you’ll need to stop using them before your evaluation. Soft lenses should be avoided for at least one week, while rigid gas-permeable lenses require a break of at least three weeks. This allows your cornea to return to its natural shape, ensuring the most accurate measurements. Once you’re confirmed as a candidate, the clinic uses advanced laser systems to deliver precise corrections tailored to your eyes.
Laser Vision Correction Technology
The clinic employs some of the most advanced laser systems available, specifically designed to handle complex issues like astigmatism. For instance, the VISX STAR S4 IR Excimer Laser system uses iris registration technology, which relies on high-definition cameras to track and adjust for cyclotorsion – the natural rotation of your eye when you change positions. This level of precision is crucial for achieving accurate astigmatism correction.
Additionally, the clinic uses femtosecond laser technology to create the corneal flap. This all-laser method results in thinner, more uniform flaps, which help preserve corneal tissue and reduce potential risks over time. When combined with wavefront-guided LASIK, which uses your personalized eye map to address optical aberrations, the procedure achieves exceptional accuracy. Studies using the same iDesign and VISX technology combination have shown impressive results: 83.8% of eyes with high astigmatism reached 20/20 vision or better within three months, and 90.3% were within ±0.50 diopters of their target correction.
Long-Term Care and Follow-Up
The clinic’s commitment to your vision doesn’t end with the surgery. Long-term follow-up care plays a key role in maintaining stable results from LASIK. Regular post-surgery visits are scheduled to monitor healing and ensure your vision remains stable. Right after the procedure, you’ll be advised to rest with your eyes closed for 4–6 hours and to avoid rubbing your eyes, reducing the risk of flap displacement.
To aid recovery, a combination of steroid and antibiotic eye drops is prescribed for 4–10 days. You’ll also use preservative-free artificial tears to manage dryness, which typically improves within 3–6 months. With around 96% of patients achieving 20/20 vision or better after LASIK, the procedure offers a high likelihood of long-term success and satisfaction.
sbb-itb-246add9
Does LASIK last forever?
Conclusion: What to Know About LASIK for Astigmatism
LASIK provides a reliable solution for correcting astigmatism, with studies showing a safety index of 0.99 over a 10-year span. Research consistently finds that most patients achieve vision improvements ranging from 20/20 to 20/40 within months of the procedure, with many maintaining these results for a decade or longer. As Dr. Takeshi Ide, MD, PhD, explains:
"Our study shows that LASIK is an effective and safe procedure… results may represent the real-world picture of LASIK".
The success of LASIK relies on several key factors. Stable preoperative vision and precise laser alignment – achieved through wavefront-guided systems – are critical. Advanced technology plays a crucial role. For instance, wavefront-guided LASIK with iris registration systems can correct for cyclotorsion, the natural rotation of the eye when lying down. Even a small misalignment of 10° could lead to a 35% undercorrection of astigmatism.
A practical example of this approach is seen at Cheyenne Eye Clinic and Surgery Center, where iDesign Advanced WaveScan mapping and VISX STAR S4 IR laser technology are used to deliver consistent results. Their process includes rigorous patient screening, precise all-laser flap creation, and thorough follow-up care, aligning with research-backed factors for long-term success.
While a small percentage of patients (around 35.8%) may require retreatment within 10 years, overall satisfaction rates remain high, ranging from 92% to 95%. When paired with modern technology and careful patient selection, LASIK continues to be a dependable option for treating astigmatism effectively and safely.
FAQs
How effective is LASIK for correcting astigmatism in the long term?
LASIK has shown impressive results in providing long-term correction for astigmatism. Studies reveal that more than 90% of patients achieve 20/20 vision or better, even a decade or two after undergoing the procedure. Many individuals express satisfaction with the significant improvement in their vision.
The procedure is both safe and dependable, with modern advancements in technology improving results and minimizing potential risks. If you’re thinking about LASIK, it’s important to speak with a trusted eye care professional to see if it’s a suitable choice for your needs.
What recent advancements in LASIK technology have enhanced its effectiveness for astigmatism?
Recent developments in LASIK technology have taken astigmatism correction to a whole new level. Wavefront-guided LASIK stands out by customizing treatments to match the specific details of each patient’s eye. This personalized approach leads to sharper, more precise vision correction. On top of that, advanced laser systems – built for high-speed accuracy – have proven highly effective in addressing mixed astigmatism, all while prioritizing safety and patient comfort.
These advancements not only enhance visual clarity but also help minimize potential side effects, making LASIK an even more dependable solution for managing astigmatism over the long term.
What makes someone a good candidate for LASIK surgery?
Determining whether LASIK is a good fit for you depends on a few key factors, including your prescription stability, the condition of your cornea, and your overall eye health. Ideally, candidates should have had a stable prescription for at least a year since fluctuations in vision can affect the procedure’s success. Additionally, the cornea must have sufficient thickness to safely handle the reshaping process. Certain conditions, like keratoconus, severe dry eye, or other eye diseases, may rule out LASIK as an option.
Age also plays a role – most people considering LASIK are at least 18 years old, as vision changes are more likely in younger individuals. To determine if LASIK is safe and appropriate for you, a comprehensive evaluation by an eye care professional is essential. This assessment ensures the procedure aligns with your specific eye health and vision needs.
